Dr. Eshika Dubey
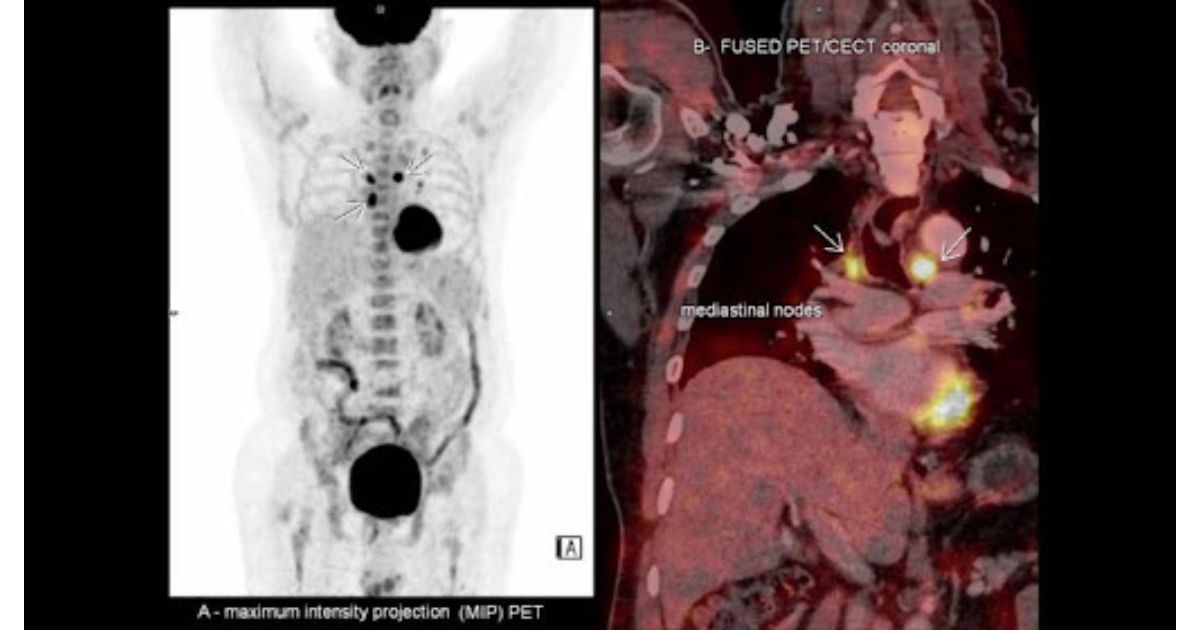
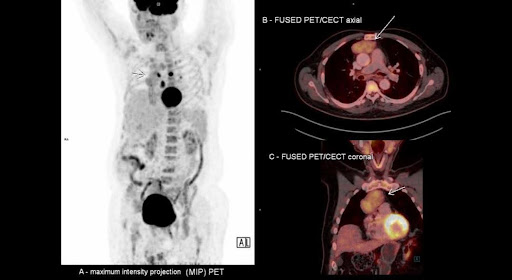
This whole-body FDG-PET scan of a patient reveals diffuse, moderately increased FDG uptake in a well-defined, heterogeneously hypo-enhancing mass with lobulated borders located in the right prevascular region. The mass measures approximately 3 x 5.5 x 7 cm, with slight bulging along the right mediastinal border, suggesting a possible thymic neoplasm. Additionally, there is evidence of high-grade FDG uptake in enlarged, mildly enhancing lymph nodes in the left lower paratracheal (largest node measuring 18 x 14 mm), right tracheobronchial, subcarinal, and left hilar regions, raising the suspicion of a granulomatous etiology in the context of known CVID. The presence of increased metabolic activity in the para-sinus areas also indicates ongoing inflammatory processes.
Differential Diagnosis:
- Thymoma
- Thymoma-associated hypogammaglobulinemia (Good’s Syndrome)
- Neurogenic tumors
- Benign cysts
- Lymphadenopathy (LAD)
- Lymphomas
- Thyroid masses
Why might this be Good’s Syndrome, and how is it diagnosed?
Good’s syndrome is a rare adult-onset immunodeficiency disorder characterized by the triad of thymoma, hypogammaglobulinemia, and increased susceptibility to recurrent infections. It typically presents in individuals during their 4th or 5th decade of life, with the average age of diagnosis around 62–65 years. Patients often present with an asymptomatic anterior mediastinal mass, although symptoms such as cough, chest pain, dysphagia, dyspnea, and hoarseness may develop due to thymoma. Additionally, Good’s syndrome can be associated with superior vena cava syndrome, Horner’s syndrome, and neck masses.
Diagnosis is frequently made during investigations for conditions like Myasthenia Gravis, with which Good’s syndrome has a significant association. Immunological findings in Good’s syndrome include hypogammaglobulinemia, a decreased or absent B cell count, abnormal CD4+:CD8+ T cell ratios, CD4+ T cell lymphopenia, and impaired T cell responses, along with reductions in serum IgG, IgA, and IgM levels. The disease shares features with X-linked agammaglobulinemia (XLA) and common variable immunodeficiency (CVID).

Patients with Good’s syndrome may experience recurrent bacterial infections (e.g., urinary tract, skin infections), as well as opportunistic infections, such as cytomegalovirus (CMV) colitis, retinitis, and mucocutaneous candidiasis. It is important to suspect Good’s syndrome in individuals over 40 years of age who have a suspected or confirmed antibody deficiency, especially when they present with such infections and reduced mature B cell counts. This suspicion is further heightened in patients with presumed CVID attending immunology clinics. One of the first diagnostic steps in such cases is to measure serum immunoglobulins. A reduction in immunoglobulins, along with a history of sinopulmonary or opportunistic infections, is crucial in diagnosing Good’s syndrome.
Treatment
The primary treatment for thymoma is surgical removal or debulking of the tumor. For patients with stage 3 or 4 thymomas, radiotherapy and/or combination chemotherapy may be necessary. Immunoglobulin replacement therapy is required to address the antibody deficiency. If the patient has a CMV-negative or unknown CMV serology, CMV-negative blood products should be administered to avoid the risk of iatrogenic CMV infection.
Author’s Biography
Dr. Eshika Dubey, an MBBS doctor currently working in Paediatrics at HBT Cooper Municipal Hospital. She has experience in Nuclear Medicine from HN Reliance Hospital and aspires to specialize in Radiology or Dermatology in the UK. She is a graduate of MGM Medical College and is interested in unique cases, research and writing.